 |
 |
 |
| Neil Ferguson, Ph.D. | Infamous Graph | Youyang Gu |
D. Joy Riley, M.D., M.A.
Executive Director
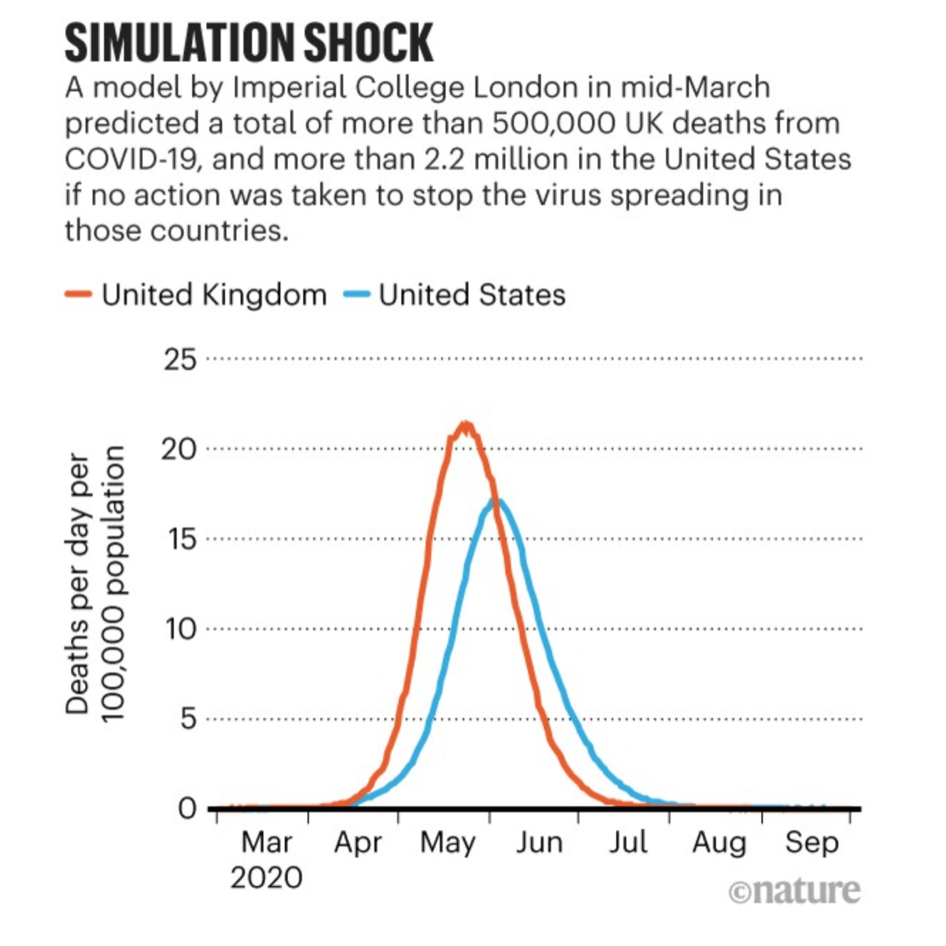
It was a long year ago (March 2020) that a dire prediction was issued by a group at Imperial College London (UK) regarding the possible effects of the novel coronavirus, SARS-CoV-2. The model predicted more than 500,000 UK deaths, and >2.2 million deaths in the U.S. by summer if no action were taken. One of the data scientists issuing that proclamation was Neil Ferguson, Ph.D. He and his group advised the government that “in the UK and US context, suppression will minimally require a combination of social distancing of the entire population, home isolation of cases and household quarantine of their family members. This may need to be supplemented by school and university closures, though it should be recognised that such closures may have negative impacts on health systems due to increased absenteeism. The major challenge of suppression is that this type of intensive intervention package – or something equivalently effective at reducing transmission – will need to be maintained until a vaccine becomes available (potentially 18 months or more).”
Ferguson’s area of expertise is the spread pattern of infectious diseases in both humans and animals. He has previously used mathematical modelling to evaluate several outbreaks of disease:
2001 foot-and-mouth disease in the UK (he was knighted for this work)
2009 swine flu in the UK
2012 MERS (Middle East respiratory syndrome – a coronavirus) outbreak
2016 Ebola in Western Africa
Importantly, Ferguson is also an International Member of the US National Academy of Medicine.
Shortly after his dire warnings, Neil Ferguson contracted SARS-CoV-2, and “completely isolated (himself) for almost two weeks after developing symptoms.” Then he broke the rules: The 51-year-old professor asked his (married) “mistress Antonia Staats, 38, to travel across London to his home at least twice during the peak of the outbreak.” He was neither fined nor prosecuted for breaking the lockdown rules, but he did resign at least temporarily (a week?) from SAGE, a UK government advisory panel. The Guardian reported in December 2020 on the effects of the pandemic and the data scientist’s experience in it: “Perhaps not surprisingly, Ferguson says that he has struggled to switch off or engage with friends and family.”
Imperial College London was not the only source of modelling and projection last spring. Another source was the Institute for Health Metrics and Evaluation, or IHME, based in Seattle. That center’s forecast was far more conservative, predicting about 60,000 deaths in the U.S. by August.
Why were the predictions so incredibly varied? Could either be believed? Was there a better model? Enter Youyang Gu, a young Chinese immigrant who had grown up in Illinois and California. Bloomberg News described Gu as having a “master’s degree in electrical engineering and computer science from the Massachusetts Institute of Technology and another degree in mathematics, but no formal training in a pandemic-related area such as medicine or epidemiology.”
He did have experience in both financial data sets and sports analytics, however, and thought he could be successful in pandemic assessment. While living with his parents in Santa Clara, Calif., Gu spent a week in April building a Covid death predictor and website. It was a relatively simple model. He noted that Covid tests, hospitalizations, and other factors were being reported inconsistently by states and the federal government, and that the most reliable figures appeared to be the daily death counts. So he stuck with that single data point, and using machine learning algorithms, kept honing his model.
Gu put in the same number of hours he would have worked at a full-time job, but notably according to Bloomberg, he “volunteered his time and lived off his savings. He wanted his data to be seen as free of any conflicts of interest or political bias.” Bloomberg News further notes that, “While certainly not perfect, Gu’s model performed well from the outset. In late April he predicted the U.S. would see 80,000 deaths by May 9. The actual death toll was 79,926. A similar late-April forecast from IHME predicted that the U.S. would not surpass 80,000 deaths through all of 2020. Gu also predicted 90,000 deaths on May 18 and 100,000 deaths on May 27, and once again got the numbers right.”
Although he initially had difficulty getting attention, he persisted in e-mailing epidemiologists and flagging his model to reporters on Twitter. Finally, a prominent biologist tweeted about Gu’s model near the end of April, and the CDC took note. Gu joined “teams of professional modelers and epidemiologists” in regular meetings of the CDC. “Traffic to Gu’s website exploded, with millions of people checking in daily to see what was happening in their states and the U.S. overall.”
“A month before stopping the COVID-19 death forecast project in November 2020, Gu had predicted that the U.S. would record 231,000 deaths on Nov. 1. When Nov. 1 arrived, the U.S. reported 230,995 deaths.” Gu was not finished, however. He added a “Path to Herd Immunity” page in December 2020, because he “felt that there were too many unfounded claims and misinformation being floated around regarding the vaccine (e.g. calculations that completely ignore immunity acquired from natural infection).”
A blog entry on 26 February 2021 includes these words from Youyang Gu:
“My goal when I started covid19-projections.com was to create the most accurate COVID-19 model. I continued the project for the next year because I saw a striking need for an unbiased, unpolitical, data-driven take of the pandemic. I feel incredibly fortunate to be in the situation I am today. I have made countless mistakes, but each one has taught me to be a better scientist. I’m thankful that I was able to use my skillset to help improve our understanding of this pandemic. A year ago, I could not have remotely imagined that I would be where I am today. I am also extremely grateful for the work of scientists whose dedicated research I’ve relied on over the past year. Science is and will always be a collaborative effort – no single person’s work stands alone.”

Virtue Ethics:
More Than Ticking a Box
C. Ben Mitchell, Ph.D.
Distinguished Fellow
Standard accounts of ethics often focus on the behavior of the decision maker: whether to act according to a certain rule, maximize the greatest good for the greatest number, or some other moral principle. This approach is not without merit and assuredly ethical systems should provide some guidance for action. Yet the focus on principles or rules fails to address a prior question, namely, what is the motivation of the decision maker to do the right thing? Why should he or she follow the rules?
If professional ethics in health care is merely about following the rules, then robots will take all those jobs. An artificial intelligence can be programmed to follow the rule perfectly, every time. But ethics is not mere compliance. Ethics is also about the character of the decision maker.
A medical professional is a person whose character has been shaped by practices that shape moral formation. The practice of doing the right thing for the right reasons cultivates virtuous character, developing the habit of ethical propriety.
Unfortunately, as soon as one appeals to notions like propriety, virtue, and character, someone will trot out that old saw, “but what’s true for you may not be true for me” or “everyone has their own set of beliefs about right and wrong.” These retorts are often meant to be conversation stoppers used to avoid awkward discussions of religion or politics.
It turns out that there is amazing universality about the shape of a person of virtuous character, as the following table will show:
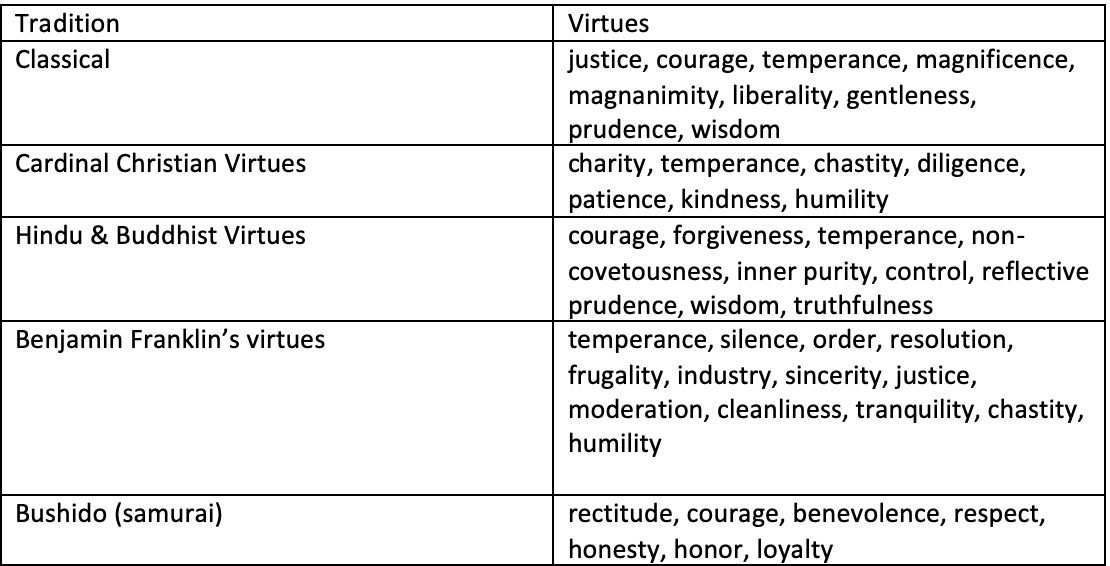
What this simple illustration demonstrates is that despite some cultural differences of mores and codes of this, there is near unanimity about the shape of virtuous character.
Medical professionals are held to high moral standards not primarily for legal and political reasons, but because of the trust put in them by patients and communities. As Drs. Edmund Pellegrino and David Thomasma, the late pioneers of 20th century medical ethics have said, “Medicine is a moral community because it is at heart a moral enterprise and its members are bound together by a common moral purpose. If this is so, they must be guided by some shared source of morality—some fundamental rules, principles, or character traits that will define a moral life consistent with the ends, goals, and purposes of medicine” (The Virtues of Medical Practice, Oxford University Press, 1993).

