
Joyce A. Shelton, Ph.D.
Professor of Biology Emerita
Trinity International University
Successful xenotransplantation, animal donor to human recipient organ transfer, is the holy grail for medical doctors and scientists who study organ transplant. Why? Approximately 107,000 people are awaiting organ transplant in the US. Most will wait up to 2 to 3 years. About 17 people die per day because there are not enough organs available to meet the demand (1). Animal organs that have been genetically engineered to remove tissue molecules that cause transplant rejection would go a long way toward relieving the organ shortage.
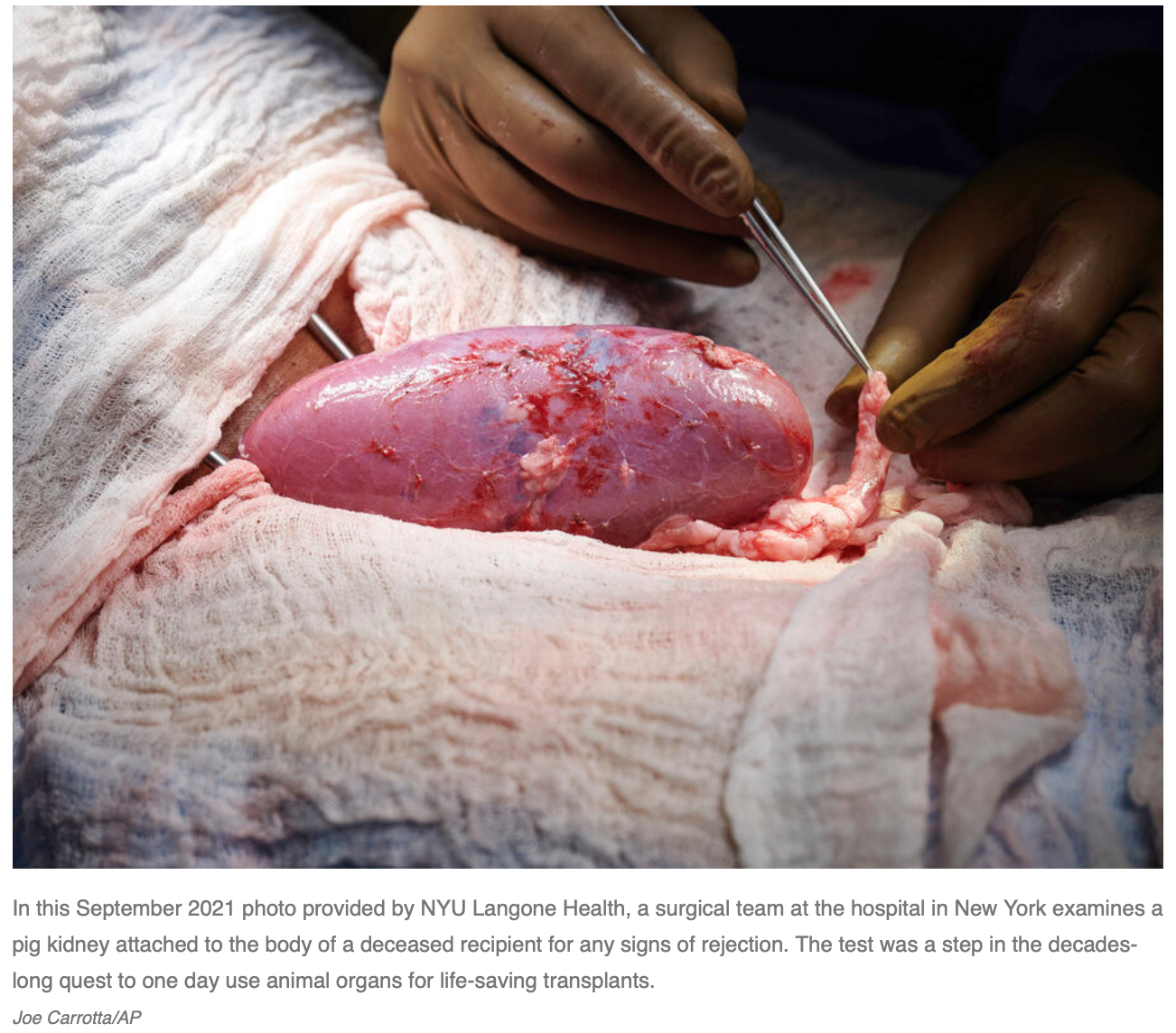
A recently proclaimed major transplantation breakthrough attracted widespread media coverage. A group of doctors at NYU Langone Health successfully attached a pig kidney to a brain dead person and showed that it could function for 54 hours without being rejected. A sugar molecule known to cause immediate rejection had been genetically removed from the pig organ (2, 3, 4). The researchers passionately predicted that their achievement could lead to patients receiving pig kidneys in “the next year or two” (5). Regardless of the sensationalism, many scientists were not overly impressed by the report. Instead, they wondered what of significance was learned from an experiment on one human being (6). The bigger challenge is overcoming chronic long term rejection of transplants, rather than immediate rejection responses already shown to be controllable (7). This experiment seemed more about fame than altruism.
Perhaps the media hype would have better been focused on the doubtful ethics of this study. The researchers would likely refer us to a published ethical analysis of their experiment by Arthur Caplan, a well-known bioethicist, and colleague Brendan Parent, both employed by NYU Langone Health. They concluded, predictably, that no ethical boundaries were breached (8). Desperately needed, before these medical celebrities continue to move forward, is a deliberative, broad public discussion of the ethical concerns.
Xenotransplantation scientists and ethicists agree that ethical guidelines are still needed (9). Additionally, the use of brain dead bodies for experimentation has been quietly happening with little or no regulation (10, 12). This lack of ethical guidance melds in the recent experiment. The AMA has direction for dealing with live and cadaver donations of organs (11); but, this was not an organ donation. There are no guidelines for using a brain dead individual’s body to test animal organs. Likewise, while there are provisions for consent by individuals to donate their organs after death, there are none for consent to use one’s body as a human test tube for in vitro (or perhaps the term should be in vivo) study of an animal organ transplant. Research ethics laws protect living human subjects. They do not apply to the human creatures we have created by technologically keeping the body alive after the brain is deemed no longer functional, subjects who are considered to be “dead” (12). Given that criteria used for brain death are varied and vague (13, 14), the moral status of a brain dead individual is not straightforward. At the very least such individuals deserve an opportunity, similar to that offered to organ donors, to decide for themselves if they want their bodies to be kept alive and utilized in this less than dignified way. Surrogates under pressure may not make the wisest decisions (15). The recently declared brain dead and also the medically vulnerable individuals who are so desperately waiting for kidney transplants that they are willing to try any hopeful remedy warrant our immediate concern. They would be the logical guinea pigs for any clinical trials of pig organ transplants in the near future. Despite the quest to be first to demonstrate successful organ transplant options for the medically needy, the welfare and dignity of all the human subjects in this drama, body donors or organ recipients, should be protected.
The Tennessee Center for Bioethics & Culture encourages respectful discussion and debate of bioethics issues, and strongly supports freedom of speech. To that end, we invite and welcome other voices to the discussion of bioethics issues. Invited authors’ views are their own, and do not necessarily represent those of The Tennessee Center for Bioethics & Culture.
References
1. https://www.organdonor.gov/learn/organ-donation-statistics. Retrieved Oct. 27, 2021.
2. https://www.cbsnews.com/news/pig-kidney-transplant-human-patient/. Retrieved Oct. 22, 2021.
3. Michelle Roberts, Pig kidney transplant to human: Surgeons pass pig kidney transplant test to brain-dead human; BBC News online, Oct. 21, 2021. Retrieved Oct. 22, 2021.
4. https://www.theguardian.com/society/2021/oct/20/pig-kidney-animal-human-transplant-us-trial. Retrieved Oct. 22, 2021.
5. https://wtop.com/lifestyle/2021/10/successful-pig-to-human-kidney-transplant-a-transformative-moment/; CBS News, Oct. 20, 2021. Retrieved Oct. 22, 2021.
6. Jason Mast, No, scientists are not any closer to pig-to-human transplants than they were last week; Endpoints, Oct. 22, 2021.
7. Malgorzata Kloc and Rafik Ghobrial, Chronic allograft rejection: A significant hurdle to transplant success, Jan. 26, 2014; doi:10.4103/2321-3868.121646.
8. Arthur Caplan and Brendan Parent, The ethics of saving lives through a new type of organ transplant; New York Daily News, Oct. 25, 2021. Retrieved Oct. 26, 2021.
9. Wayne Hawthorne, et al., Third WHO Global Consultation on Regulatory Requirements for Xenotransplantation Clinical Trials; Changsha, Hunan, China; Dec. 12–14, 2018.
10. L Yasko, M Wicclair, and M DeVita, Committee for Oversight of Research Involving the Dead (CORID): Insights from the First Year; Cambridge Quarterly of Healthcare Ethics, 2004; 13(4), 327-337; doi:10.1017/S096318010413404X.
11. https://www.ama-assn.org/sites/ama-assn.org/files/corp/media-browser/code-of-medical-ethics-chapter-6.pdf. Retrieved Oct. 27, 2021.
12. https://www.reliasmedia.com/articles/484-research-on-the-dead-standards-are-required, Mar. 1, 2004. Retrieved Oct. 27, 2021.
13. DM Greer, HH Wang, JD Robinson, PN Varelas, GV Henderson, and EFM Wijdicks, Variability of Brain Death Policies in the United States. JAMA Neurology, 2016; 73(2):213–218; doi:10.1001/jamaneurol.2015.3943.
14. Erin Barnes and David Greer, Inconsistency in Brain Death Determination Should Not Be Tolerated; AMA J Ethics, 2020; 22(12):E1027-1032.; doi: 10.1001/amajethics.2020.1027.
15. Joseph Fins, Disorders of Consciousness and Disordered Care: Families, Caregivers, and Narratives of Necessity; Archives of Physical Medicine and Rehabilitation, 2013; 94:1934-9.
