D. Joy Riley, M.D., M.A.
Executive Director

As a teenager, I decided I wanted to be a physician — to help people. I also naively thought that medicine was apolitical. I should have read more history. If I had, I might have come across the story of Ignác Fülöp Semmelweis.
Semmelweis was born to Hungarian parents slightly more than 200 years ago, in 1818. Although he began to study law, he ended up graduating from medical school in 1844. Other plans of his changed as well. When he did not land a position in internal medicine, he spent four extra months training to become an obstetrician. He actually received a “master’s diploma in practical midwifery” (Baskett, 201). He is known for his groundbreaking work on prevention of puerperal (“childbed”) fever. He is also known for being vilified for his work on puerperal fever.
In 1846, Semmelweis, who, in addition to obstetrics, had experience in pathology and statistics, was appointed as an assistant to Professor Johann Klein at Vienna’s Allgemeines Krankenhaus (Vienna General Hospital). This same professor Klein had earlier “instituted autopsy teaching for students” (Ibid., 202). There were two obstetrical clinics of the Vienna General Hospital in July of 1846. Medical students were instructed in the First Clinic; the Second Clinic was for midwives only.
Maternal mortality rates in Vienna were not that different from other locales at the time (Hellman, 34). Yet there was a difference between the First and Second Clinic rates. Noting the higher rate of maternal mortality in the First Obstetrical Clinic compared to the Second Clinic, Semmelweis examined the records dating back to 1794. It was after the inclusion of autopsy training for medical students and physicians that the death rate rose, and the difference between the two clinics was more remarkable after 1840, when the medical and midwifery trainees were separated between the two clinics.
More evidence for an external source for puerperal sepsis came in a personally painful manner. Semmelweis’ colleague, Kolletschka, suffered an accident. A medical student accidentally punctured his professor’s skin at an autopsy, and Kolletschka died from sepsis. His course mirrored the disease course of the women dying of puerperal sepsis. There must be something carried from the dead bodies to the obstetrical patients — on the hands of the medical students and doctors.
In May, 1847, Semmelweis instituted hand washing with “chloride of lime” for all medical students and doctors who entered the maternity ward. “Within one month the mortality in the first division fell from 12.2 per cent to 2.4 per cent. In 1848, the first full year of chlorine prophylaxis, the death rate in the first division fell to 1.2 per cent, comparable to the 1.3 per cent in the second division” (Baskett, 202).
Semmelweis needed to tell everyone about this! Some of his supporters tried to help get out the message, but others obstructed his way. Professor Klein was one of the latter. He influenced others to prevent review of the findings, and “refused to reappoint Semmelweis in March 1849” (Ibid., 202). It was finally in 1860 that Semmelweis published his work. History has proven him correct both in his understanding of the problem and in his efforts to avert it.
Approximately half a century after Semmelweis’ discovery, George Santayana (1863-1952) wrote “Those who cannot remember the past are condemned to repeat it” (in The Life of Reason; see quote here).
Consider recent events. On 4 October 2020, a declaration was signed by three infectious disease epidemiologists and public health scientists recommending a strategy for dealing with COVID-19. The Great Barrington Declaration (GBD) promoted “Focused Protection” of the vulnerable while allowing those “at minimal risk of death to live their lives normally” as herd immunity was being attained.
Drs. Martin Kulldorff (Harvard), Sunetra Gupta (Oxford), and Jay Bhattacharya (Stanford) wrote in part:
Coming from both the left and right, and around the world, we have devoted our careers to protecting people. Current lockdown policies are producing devastating effects on short and long-term public health. The results (to name a few) include lower childhood vaccination rates, worsening cardiovascular disease outcomes, fewer cancer screenings and deteriorating mental health – leading to greater excess mortality in years to come, with the working class and younger members of society carrying the heaviest burden. Keeping students out of school is a grave injustice.
Keeping these measures in place until a vaccine is available will cause irreparable damage, with the underprivileged disproportionately harmed.
Fortunately, our understanding of the virus is growing. We know that vulnerability to death from COVID-19 is more than a thousand-fold higher in the old and infirm than the young. Indeed, for children, COVID-19 is less dangerous than many other harms, including influenza.
As immunity builds in the population, the risk of infection to all – including the vulnerable – falls. We know that all populations will eventually reach herd immunity – i.e. the point at which the rate of new infections is stable – and that this can be assisted by (but is not dependent upon) a vaccine. Our goal should therefore be to minimize mortality and social harm until we reach herd immunity.
The most compassionate approach that balances the risks and benefits of reaching herd immunity, is to allow those who are at minimal risk of death to live their lives normally to build up immunity to the virus through natural infection, while better protecting those who are at highest risk. We call this Focused Protection.
On 8 October 2020, Gregg Gonsalves wrote “Focused Protection, Herd Immunity, and Other Deadly Delusions” in The Nation.
On 14 October, NIH director Francis Collins responded to the GBD in this quote by the Washington Post:
“What I worry about with this is it’s being presented as if it’s a major alternative view that’s held by large numbers of experts in the scientific community. That is not true,” Collins, NIH director, said in an interview.
“This is a fringe component of epidemiology. This is not mainstream science. It’s dangerous. It fits into the political views of certain parts of our confused political establishment,” he said. “I’m sure it will be an idea that someone can wrap themselves in as a justification for skipping wearing masks or social distancing and just doing whatever they damn well please.”
On 6 November 2020, an opinion piece by a public health professor at Syracuse University, Brooks B. Gump, was published in U.S. News & World Report: “The Great Barrington Declaration: When Arrogance Leads to Recklessness.”
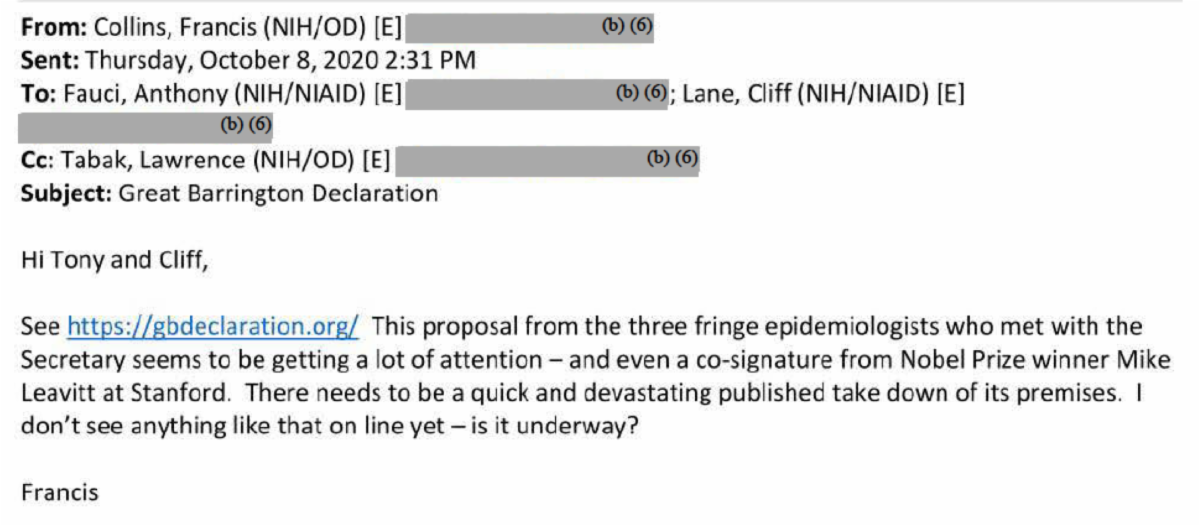
These publications critical of the Great Barrington Declaration are not the only ones — not at all. It is informative to note that an email obtained through a Freedom of Information Act request, obtained by the American Institute for Economic Research, shows some planning of a public takedown of the Great Barrington Declaration and its authors. Here is a screenshot of that email:
Whatever the outcome of the COVID-19 policies, and we are living with the aftermath of many, we all need to read more history. In the meantime, we can all work at being more charitable toward one another.
References
1. Baskett, Thomas F. “Semmelweis, Ignac Philipp (1818-1865): Puerperal Sepsis.” Essay. In On the Shoulders of Giants: Eponyms and Names in Obstetrics and Gynaecology, 201–3. London, England: RCOG Press, 2001.
2. Hellman, Hal. “Semmelweis versus the Viennese Medical Establishment.” Essay. In Great Feuds in Medicine Ten of the Liveliest Disputes Ever, 33–51. New York, NY: John Wiley & Sons, 2001.